Part 8: Specific Joint and Soft Tissue Pathology
ASSESSMENT OF JOINTS
Rheumatoid arthritis
Typically involves metatarso-phalangeal joints in a bilateral symmetrical fashion
Early findings are soft tissue swelling, joint effusions and periarticular osteoporosis
Progressive joint space narrowing and periarticular erosions as synovial pannus invades cartilage and bone
Generalised osteoporosis and characteristic valgus deformities of the toes progressing to gross subluxation and dislocation in severe cases
Midtarsal and hindfoot involvement is present in long-standing cases
In juvenile disorders such as Still’s disease there may be epiphyseal overgrowth and early fusion with delayed long bone growth and ‘spindling’ of the digits

Rheumatoid arthritis with symmetrical MTP joint loss, erosions and subluxation
Osteoarthritis
Narrowing and irregularity of joint space
Damaged cartilage may become calcified (chondrocalcinosis)
Subarticular sclerosis with subchondral cysts Osteophytes
Bone density usually maintained
In late stages, the joint becomes partially or fully ankylosed and osteophytes may fracture, causing loose intra-articular bodies

Osteoarthritis of the 1st MTP joint with joint space narrowing, subarticular sclerosis and marginal osteophytes (arrows)
Gout
Hyperuricaemia causes deposition of urate crystals
First metatarso-phalangeal joint is commonly involved, termed a podagra
Well-defined erosions with sclerotic borders which have a ‘punched out’ or ‘rat bite’ appearance and overhanging margin
Joint space and bone density are preserved until late in the course of the disease
Urate crystals deposited in the soft tissues form tophi and periarticular lobulated soft tissue masses
Chondrocalcinosis may represent deposition of calcium pyrophosphate dihydrate (CPPD) crystals (pseudogout)

Gout of first MTP joint with well defined ‘punched out’ erosion with overhanging margin (arrow) and soft tissue swelling (arrowheads)
Sero-negative spondyloarthropathy
Includes ankylosing spondylitis, psoriasis and Reiter’s syndrome; linked to HLA B27 antigen complexes
Usually involves interphalangeal joints in an asymmetrical distribution
Soft tissue swelling leads to dactylitis or ‘sausage digits’
Loss of joint space and ill-defined erosions with proliferative new bone formation and periostitis
Erosion of bone end into a sharpened pencil shape giving a ‘pencil in cup’ deformity
Severe forms progress to ankylosis
Fluffy new bone formation and erosions may occur at the calcaneal insertions of the Achilles and plantar fascia

Psoriatic arthropathy with new bone proliferation (arrowhead) and ‘pencil in cup’ appearance (arrow)
Synovial osteochondromatosis
Occurs mainly in young or middle-aged adults
Multiple metaplastic cartilaginous bodies form in the synovial membrane of a joint and become ossified
Seen as multiple calcified intra-articular bodies, accompanied by a joint effusion
In chronic cases, there may be pressure erosion of the periarticular bone

Synovial osteochondromatosis of the ankle joint with multiple intra-artcular ossific bodies (arrows)
Pigmented villonodular synovitis
More recently called intra-articular tenosynovial giant cell tumour
Most commonly seen in young adults
Characterized by villous nodular proliferation of the synovium with haemosiderin deposition
Dense periarticular soft tissue swelling with pressure erosion of the subarticular bone
Joint space preserved until fairly late
No calcification
MRI useful to demonstrate the villous nodular synovial masses with low signal haemosiderin on all imaging sequences

PVNS with periarticular soft tissue swelling (arrowheads), bone erosion (arrow) and low signal synovial proliferation on MRI (arrows)
Septic arthritis
Subchondral osteopenia due to hyperaemia
Joint effusion with displacement of periarticular fat planes
Rapid destruction of joint space
Radiolucency and bone destruction on both sides of the joint

Septic arthritis 1st MTP joint with soft tissue swelling (arrows), loss of joint space, periarticular lucency and early osteolysis

Septic arthritis 3rd MTP joint with rapid loss of joint space and periarticular bone destruction (arrows)
ASSESSMENT OF SOFT TISSUES
Soft tissue mass
Soft tissue mass identified on plain radiograph with distortion of soft tissue contours and increased density
May require further evaluation with ultrasound and/or MRI

Soft tissue mass at the first MTP joint (arrowheads) corresponded to a ganglion confirmed on USS

Posterior ankle soft tissue swelling confirmed to be Achilles xanthomatosis on MRI (arrows)
Soft tissue calcification
Vascular calcification has a linear ‘worm-like’ appearance, commonly seen in diabetics along the course of the dorsalis pedis artery between the first and second metatarsals
Bursal calcification is most common medial to the first metatarsal head with a hallux valgus

Bursal calcification
Post traumatic calcification within the muscles results in myositis ossificans which characteristically has dense peripheral calcification
Neoplastic calcification may be the only indication of a soft tissue mass such as a benign haemangioma (calcified phleboliths) or malignant synovial sarcoma

Haemangioma with calcified phleboliths (arrows)
Other causes of calcification include:
- collagen vascular diseases e.g. scleroderma and dermatomyositis
- metabolic disorders e.g. hypercalcaemia and gout result in soft tissue calcification
Synovial sarcoma
Synovial sarcoma is the most common malignant soft tissue tumour in the foot
Up to 16% of synovial sarcomas occur in the foot
Often presents as slow growing soft tissue mass in young adult and is often inadvertently marginally excised
May show scattered calcification in up to 50% of cases
No specific radiological features; it may be infiltrative with adjacent bone destruction but can also appear well defined; high index of suspicion is required
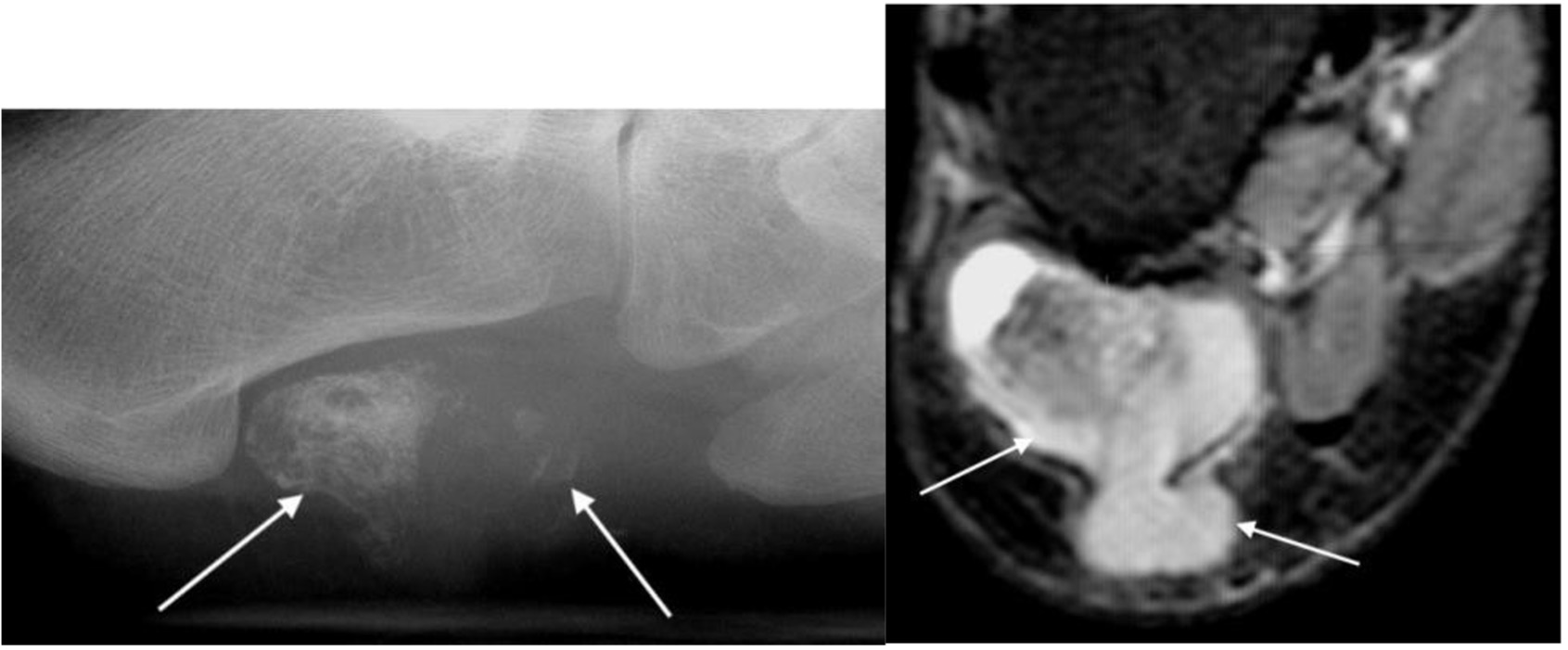
Synovial sarcoma with calcification in soft tissue mass (arrows) on plain radiograph and MRI
Foreign bodies
Radio-opaque foreign bodies seen as areas of increased density
More than one view is often necessary to locate the foreign body
Glass, plastic, thorns and wood splinters are not radio-opaque and may not be seen on radiographs; ultrasound is an excellent technique for identifying these foreign bodies which are seen as linear echogenic structures

Foreign body (arrow)