Part 4: Specific Bone Pathology:
Diabetic foot, osteochondrosis, osteochondritis dissecans
DIABETIC FOOT
Osteomyelitis
- Tends to occur at pressure points such as metatarsal heads, calcaneal tuberosity, malleoli and toes
- soft tissue changes within 3 days
- soft tissue swelling and density
- obliteration of normal soft tissue planes
- Radiolucent gas locules
- Visible bony changes may be delayed; ill-defined radiolucency and osteolysis seen at 7-14 days
- Cortical and bone destruction increases diagnostic accuracy
- Periosteal reaction as pus elevates and strips periosteum

Osteomyelitis 1st toe distal phalanx with soft tissue swelling (arrowheads), osteolysis (arrow), periostitis and increased signal on STIR (fluid-sensitive) MRI


Progressive calcaneal osteomyelitis with ill-defined radiolucency progressing to bone destruction (arrows). Skin ulcers are apparent (arrowheads)
Sequestrum = necrotic bone seen as dense sclerotic fragment due to disruption of periosteal vascular supply; may be focus of continuing infection
Involucrum = layer of periosteal new bone seen as sclerotic osseous shell encapsulating the necrotic sequestrum
Cloaca = opening in involucrum allowing drainage of pus and necrotic material
Sinus = tract extending from infected bone to skin surface
Brodie’s abscess
- Chronic, walled-off abscess containing debris and sometimes sequestrum
- Seen as radiolucent ovoid area surrounded by reactive sclerosis typically in the long bone metaphysis
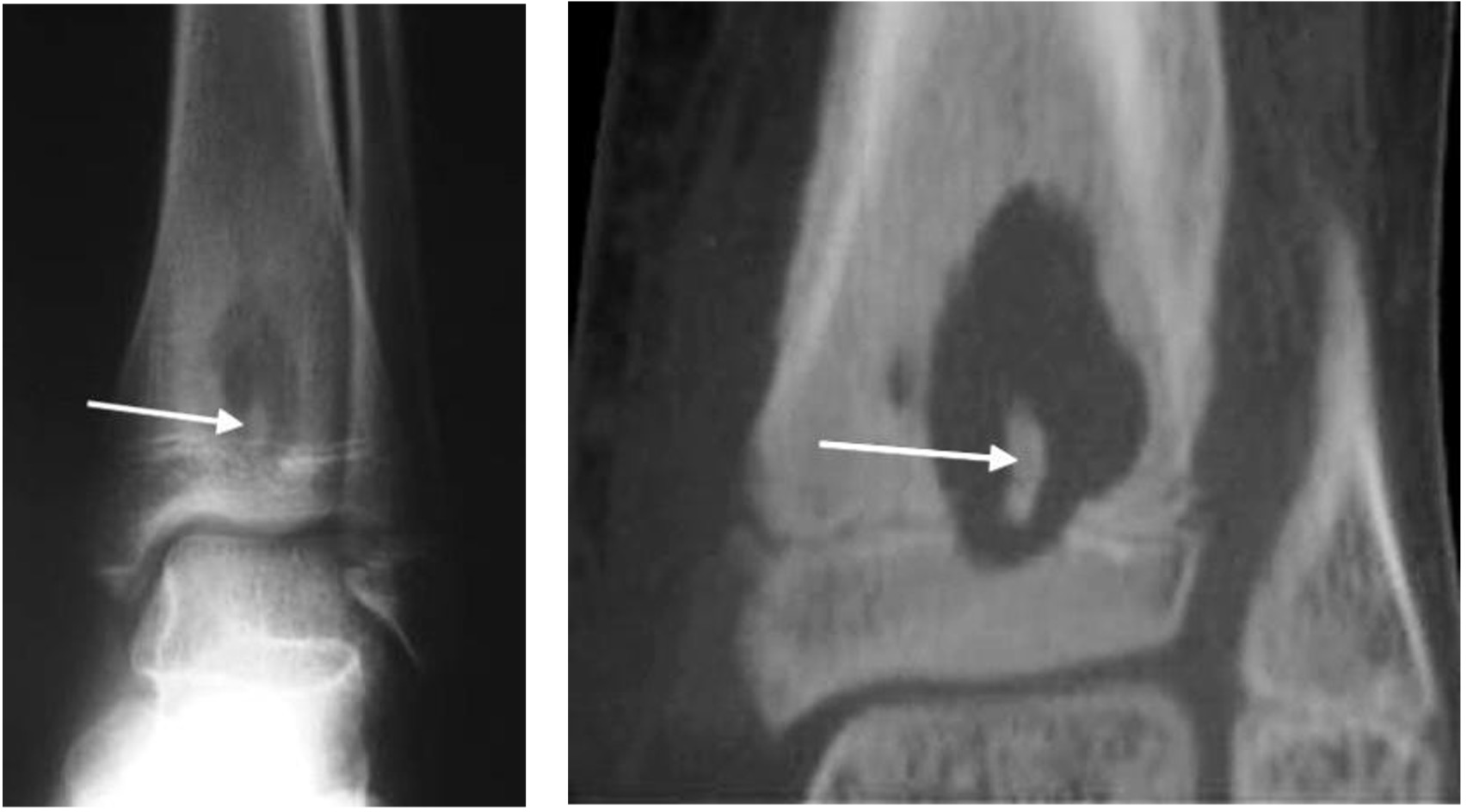
Abscess in distal tibia with sclerotic sequestrum on plain radiograph and CT (arrow)
Neuropathic or Charcot foot
Severe, destructive neuroarthropathy, often following minor or significant trauma; due to loss of sensation and proprioception. Involves the midfoot (60%), ankle (20%) or hindfoot (10%).
Radiographic features may be remembered by the following Ds:
- Dense sclerotic subchondral bone
- Degeneration
- Destruction of the joint which is often severe
- Debris which is made up of heterotopic new bone, bone fragmentation and loose bodies
- Deformity
- Dislocation (non-traumatic)
There may be minimal adjacent soft tissue abnormality.
Disease stage described using Eichenholtz classification: fragmentation, coalescence, consolidation.

Diabetic Charcot foot centred at TMT joints with dense sclerotic bone, bony debris and dislocation. Note vascular calcification (arrow).
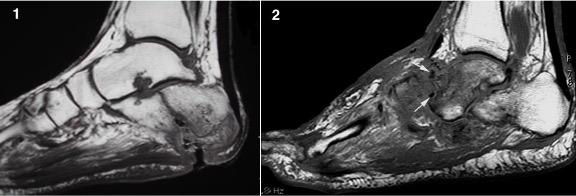
Fig 1: Osteomyelitis at calcaneal pressure point with marrow epicentre, cortical destruction and adjacent soft tissue ulcer.
Fig 2: Charcot midfoot with articular (TMTJ) epicentre, sclerotic bone fragments (arrows) and no soft tissue ulcer
OSTEOCHONDROSIS
- Term for a group of disorders that affect the immature skeleton
- Occurs in epiphysis or apophysis; includes traction apophysitis
- Aetiology possibly due to injury, repetitive trauma, overuse
- Other factors may include vascular disturbance, genetic, endocrine or mechanical
- Seen as sclerosis, flattening, irregularity and possibly fragmentation of the epiphysis
- With revascularisation, the epiphysis remodels, often with residual deformity
Freiberg’s disease
- Usually the second or third metatarsal heads
- Flattening and sclerosis of the metatarsal head
- Widening of the joint space due to the ‘eggshell crush’ degeneration of the metatarsal head
- May result in secondary osteoarthritis

Freiberg’s disease with flattening and sclerosis of the 2nd metatarsal head (arrow)
Köhler’s disease
- Involves navicular bone
- Affects ages 2–10y
- 70% of cases are in males with familial incidence
- The navicular becomes sclerotic and collapses into a disc shape (best seen on the oblique view)

Kohler’s disease with flattening and sclerosis of the navicular (arrow)
Mueller-Weiss syndrome (aka Brailsford disease)
- Although Kohler’s has been hinted as a potential cause, MWS is not truly an osteochondrosis
- Spontaneous, multifactorial, adult-onset, osteonecrosis of the navicular, 40-60y
- Sclerotic, comma-shaped navicular due to collapse of the lateral side
- Medial and/or dorsal navicular subluxation
- Lateral subluxation of the talar head, navicular split and fragmentation

Mueller-Weiss syndrome with collapse of the lateral navicular and medial navicular subluxation
Sever’s disease
- Calcaneal apophysitis, usually 8–12y. May be bilateral.
- The posterior calcaneal apophysis appears irregular and sclerotic (although these findings can be normal).
Other rarer conditions
- Iselin’s disease of the fifth metatarsal base
- Buschke’s disease of the cuneiforms
OSTEOCHONDRITIS DISSECANS
- Most common in children / adolescents
- Due to poor blood flow to subchondral bone
- Partial or complete detachment of an osteochondral fragment
- Usually involves the medial talar dome
- ‘Subchondral halo’ outlines the osteochondral fragment
- Focal flattening and compression of talar dome; osteochondral fragment within crater
- Displaced osteochondral fragment with focal concavity of talar dome and intra-articular bone fragment

Osteochondritis dissecans medial talar dome (arrow)