Malignant Tumours of the Foot
Introduction
- Very rare
- 5% of musculoskeletal tumours are foot and ankle
- Soft tissue tumours account for 25-52%
- Bone tumours account for 48-52%
- Malignant neoplasms account for 13-39%
- Bone:
- Chondrosarcoma – most common
- Osteosarcoma, Ewing’s, fibrosarcoma, metastatic
- Soft tissue:
- Synovial sarcoma, myxofibrosarcoma, malignant melanoma
- Even anatomical distribution
- Often delay in diagnosis compared to other anatomical sites
Investigations
Key history:
- Skin changes / ulceration
- Peripheral nerve compression symptoms
Key examination:
- Tinel’s sign
- Skin pigmentation changes
- Lateral and dorsal easier to diagnose than medial and plantar
- Local lymph nodes
- Pulsatility
- Tethered to underlying structures
Increased suspicion of malignancy:
- subfascial location
- lump size > 5 cm
- increase in size
- pain and /or recurrence
Radiographs
USS
- Good for soft tissue
- Defines planes
- Doppler for hypervascularity
MRI
- Whole foot
- If tibia/fibula – request whole bone to knee
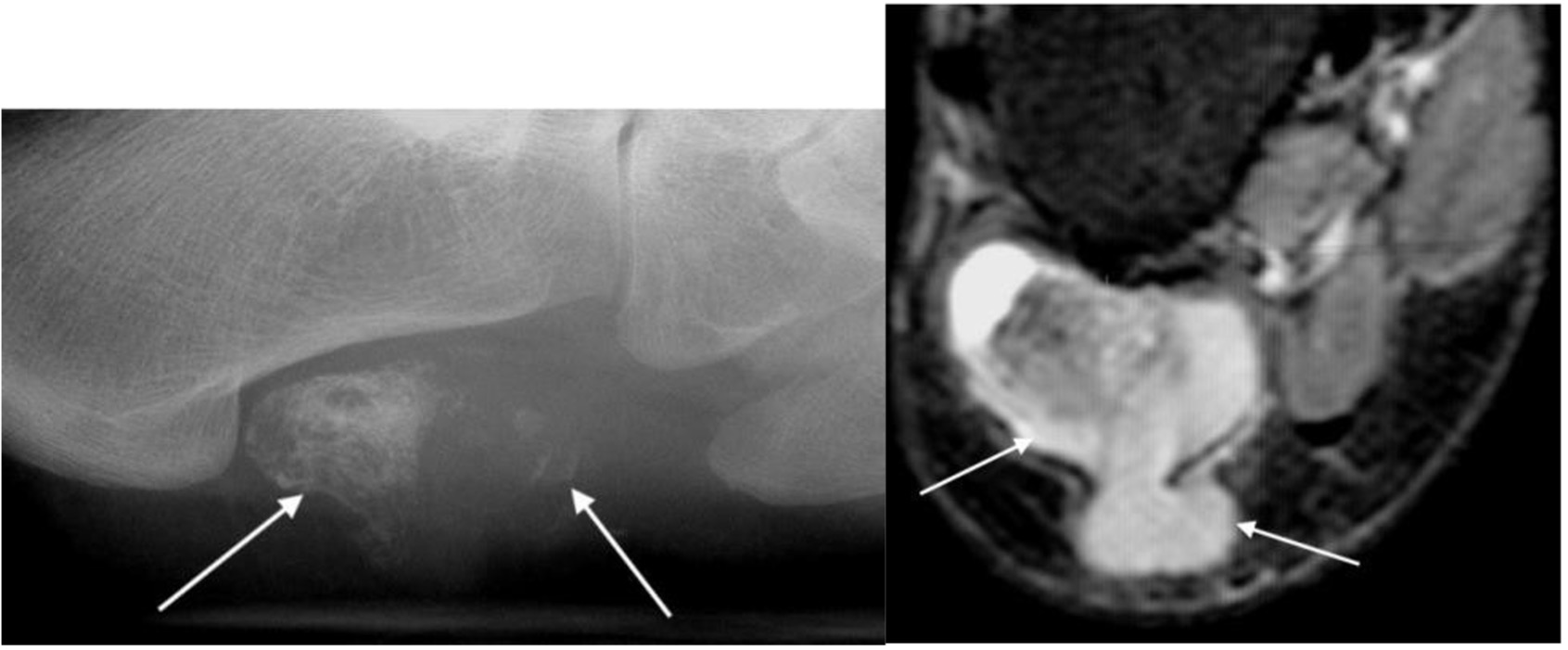
Figure 1. Xray and MRI of synovial sarcoma
CT
- Local – whole foot
- Staging – chest/abdo/pelvis
Nuclear Medicine
Management
- Early referral to local tumour / sarcoma unit
- Biopsy principles
- Only after discussion with the local tumour service / MDT discussion
- Fine needle aspiration for:
- Cytology
- Fluorescence in situ hybridization (FISH)
- PCR
- Core needle biopsy – tissue cylinder
- Open incisional
- Tumour capsule
- Cortical margin in bony tumours
Biopsy rules
- Should be same team that will perform the definite tumour resection
- Minimally invasive: access the tumour through the least possible normal tissue / compartments; avoid contact with neurovascular structures
- In line with definitive incision for later tumour resection and as far distally as possible
- Should produce sufficient and representative sample of the lesion (no necrotic or liquid components, verification by immediate frozen sections)
- Haemostasis should be performed meticulously to prevent cell spread
- If a drain is used, it must be close to – and in line with – the main incision
- Dedicated histopathologist
Management principles
- Life vs limb salvage
- MDT management
- Most malignant tumours will require a wide local excision to ensure appropriate margins
- Radical excision may mean amputation, especially in the midfoot / hindfoot; seek early input from psychological support / limb-fitting centre
- Forefoot may be amenable to ray amputation
- Know your foot amputations – ray / transmetatarsal / Lisfranc / Syme / BKA
- Work with plastic surgeons to assess soft tissue options
- Involve oncology for primary tumour management in metastatic disease
- Chemotherapy / radiotherapy
Key malignant tumours
Synovial sarcoma
- young to middle aged
- intralesional calcifications in soft tissue mass
- radical surgical excision with wide margins
- 5-year survival ~55%
Malignant melanoma
- most frequent malignant origin tumour
- commonly sole of foot
- wide excision with soft tissue coverage
- very low 5 to 10-year survival
*awaiting image upload*
Figure 2. Radiograph of malignant melanoma
Chondrosarcoma
- age: 40s – 50s
- most common malignant primary bone tumour
- hindfoot > forefoot
- irregular osseous lesion on plain radiographs
- if intermediate or high-grade, consider amputation

Figure 3. Chondrosarcoma
References
Rammelt S, Fritzsche H, Hofbauer C, Schaser KD. Malignant tumours of the foot and ankle. Foot Ankle Surg. 2020 Jun;26(4):363-370. doi: 10.1016/j.fas.2019.05.005. Epub 2019 May 11. PMID: 31126797
Hughes P, Miranda R, Doyle AJ. MRI imaging of soft tissue tumours of the foot and ankle. Insights Imaging. 2019 Jun 3;10(1):60. doi: 10.1186/s13244-019-0749-z. PMID: 31161474; PMCID: PMC6546775
Toepfer A, Harrasser N, Recker M, Lenze U, Pohlig F, Gerdesmeyer L, von Eisenhart-Rothe R. Distribution patterns of foot and ankle tumors: a university tumor institute experience. BMC Cancer. 2018 Jul 13;18(1):735. doi: 10.1186/s12885-018-4648-3. PMID: 30001718; PMCID: PMC6043962
Toepfer A. (2017). Tumors of the foot and ankle – A review of the principles of diagnostics and treatment. Fuß & Sprunggelenk. 15. 10.1016/j.fuspru.2017.03.004
Khan Z, Hussain S, Carter SR. Tumours of the foot and ankle. Foot (Edinb). 2015 Sep;25(3):164-72. doi: 10.1016/j.foot.2015.06.001. Epub 2015 Jun 10. PMID: 26233943