Freiberg’s Disease
Although the eponymous condition known as Freiberg’s disease has historically been viewed as a separate disease process, it shares all pathological features and some clinical and radiological features with AVN affecting other bones in the hindfoot.
- Most commonly seen in adolescence
- Preponderance in females
- 2nd metatarsal head most common; can be seen in 3rd
Blood Supply
Each metatarsal head has a dual blood supply:
- Medial deep plantar artery
- Dorsal metatarsal artery
Aetiology
Unknown but three broad theories:
- Trauma
- Impaired vascularity
- Systemic disorders
Trauma: repetitive micro-trauma, perhaps as a result of:
- anatomic anomaly e.g. relatively long 2nd MT compared to the 1st MT (Figure 1)
- deformity e.g. metatarsus primus varus
- inherent stability of 2nd MT due to the keystone articulation at its base
Impaired vascularity: approx 1/3 of the population may have an absent 2nd dorsal metatarsal artery ≈ possible poor watershed blood supply from neighbouring vessels
Systemic disorders: increased incidence in SLE, diabetes, hypercoagulable states; genetic?

Figure 1: DP radiographic view of a long 2nd metatarsal
Histopathology
Surgical appearances are classic of a punched out dorso-central lesion often with loose bodies and de-laminated cartilage (Figure 2). Histologically, most reports suggest a clear picture of AVN.

Figure 2: intra-operative findings of a central area of necrosis of the 2nd MT head
Clinical Picture
Pain and swelling isolated to the base of the toe. Pain may be metatarsalgic in nature or nocturnal (typical of AVN). The affected toe may be elevated form the ground, swollen and, in later stages, dislocated dorsally.
Imaging
Plain standing radiographs offer a clear diagnosis in established cases (Figure 3).
CT can help define the morphology of the MT head, especially when planning osteotomies (Figure 4).
MRI can be useful in establishing a diagnosis in earlier stages of the process.

Figure 3: established changes of Freiberg’s disease within the 3rd metatarsal head
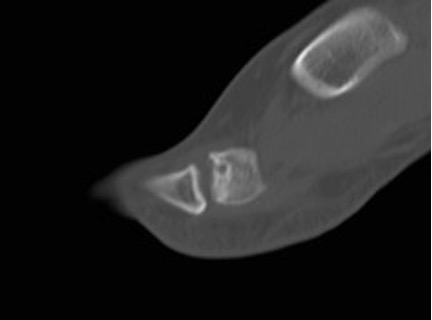
Figure 4: sagittal CT slice through the 2nd MTPJ showing the relative involvement of the dorsum of the head; this illustrates how a dorsal wedge resection osteotomy would rotate articular surface into contact with the base of the proximal phalanx
Staging
Smillie (1957) described 5 progressive stages of the disease based upon a mixture of radiographic and intra-operative findings. This staging process does not act as a tool for determining treatment.
Stage 1 - Subchondral fracture (visible only on MRI)
Stage 2 - Dorsal collapse of articular surface on plain radiographs
Stage 3 - Collapse of dorsal MT head, with plantar articular portion intact
Stage 4 - Collapse of entire MT head, joint space narrowing
Stage 5 - Severe arthritic changes and joint space obliteration
Non-operative Treatment
- Analgesia, NSAIDs
- Activity modification
- Shoe modification – stiff soles, accommodative toe box
- Orthoses – off-load the painful metatarsal head
Operative Treatment
- Core decompression – only 2 cases in the literature
- Open joint debridement
- remove loose bodies, osteophytes, and delaminated articular surface
- Metatarsal osteotomies
- dorsal closing wedge (Gauthier) – diseased area can be excised in a wedge, rotating the plantar surface into articulation with the phalanx
- shortening osteotomy (Weil type) – useful if long 2nd metatarsal
- Excision arthroplasty – risks transfer metatarsalgia and creating an unstable, short toe (Figure 5)
- Interposition arthroplasty
- rolled up EDB tendon (‘anchovy’)
- silastic replacement (Figure 6)
- more recent use of Cartiva implant with some early evidence

Figure 5: the sequelae of resecting the 2nd metatarsal head

Figure 6: pre and post-op silastic replacement
References
Carmont MR, Rees RJ, Blundell CM. Current concepts review: Freiberg’s disease. Foot Ankle Int 2009: 30(2);167-176.
Freiberg AH. Infraction of the second metatarsal bone, a typical injury. Surg Gyn Ob. 1914. 19:191.
Smillie IS. Treatment of Freiberg's infraction. Proc R Soc Med. 1967 Jan. 60(1):29-31.